Plantar fasciitis is a common and often painful condition that affects the heel. If you've ever felt a sharp pain in your heel when you take your first step in the morning, you may have experienced this condition.
Millions of people suffer from plantar fasciitis each year, especially those who stand for long periods. The condition occurs when the plantar fascia, a thick band of tissue that spans the bottom of the foot, becomes inflamed. But what causes this inflammation? And how can you prevent and manage this painful condition?
Let's learn together.
What is Plantar Fasciitis?
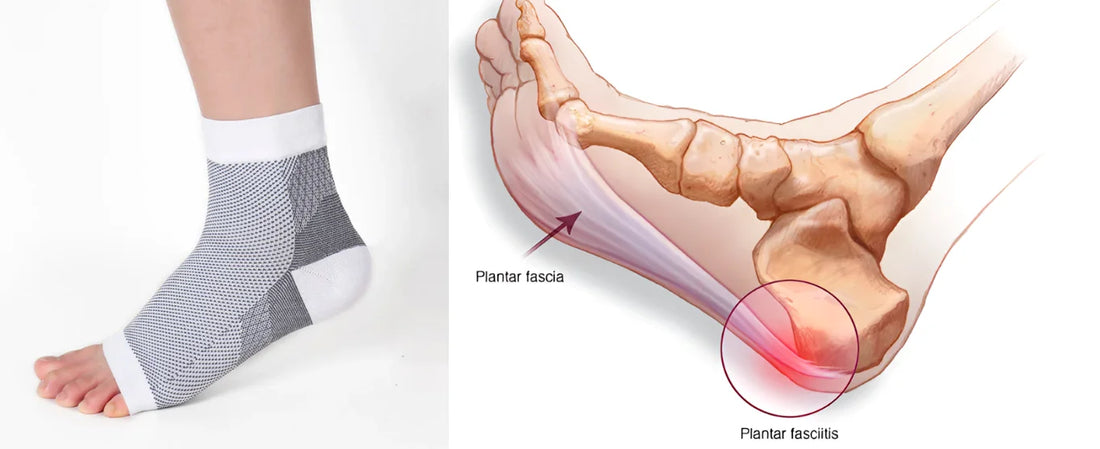
Plantar fasciitis is a common cause of heel pain. It occurs when the plantar fascia (the thick band of tissue that runs along the bottom of the foot) becomes irritated or inflamed. This inflammation usually results in a sharp, stabbing pain, especially when you take your first steps in the morning.

The plantar fascia is a strong band of fibrous tissue. It extends from the heel bone to the toes, forming the arch of the foot. Its main function is to support the arch and absorb shock as you walk. When this bundle of tissue is put under too much pressure, small tears may develop, losing some of its elasticity or toughness, and may become inflamed, leading to pain.
What Are the Symptoms of Plantar Fasciitis?
Plantar fasciitis usually announces itself with a variety of symptoms. Recognizing these early can help in managing and treating the condition more effectively. Here are the most common symptoms:
- Heel Pain: This is the most telling symptom. The pain is often sharp and intense, especially first thing in the morning or after periods of rest.
- Pain After Activity: Unlike other injuries, plantar fasciitis pain often flares up after, not during, physical activities.
- Stiffness: Many people report stiffness in the heel and the bottom of the foot, especially upon waking.
- Tenderness: The bottom of the heel might feel tender to the touch.
- Limited Mobility: The pain and stiffness can lead to difficulty in walking or exercising.
Recognizing and understanding these symptoms can help diagnose and treat plantar fasciitis early, preventing further discomfort and complications.
Causes of Plantar Fasciitis
Plantar fasciitis can be painful and limiting, but understanding what causes it can help in its prevention and treatment. Factors range from how you walk to the shoes you wear. Let's explore the main causes of this condition.
Biomechanical Factors
The way your foot moves, or your gait, can play a huge role in developing plantar fasciitis. If you have flat feet or high arches, your foot may not distribute weight evenly. This uneven distribution can put extra stress on your plantar fascia.
- Flat Feet: People with flat feet often roll their feet inward more than usual (overpronation). This puts added strain on the plantar fascia.
- High Arches: Conversely, if you have high arches, the foot can't absorb shock well. This lack of shock absorption directly impacts the plantar fascia, causing tiny tears and inflammation.
- Gait Issues: Sometimes, the way you walk can stress your feet. Abnormal walking patterns, like putting too much weight on your toes or heels, can lead to plantar fasciitis.
Lifestyle and Activity
Your daily habits and activities can significantly contribute to the development of plantar fasciitis. Certain lifestyle choices and physical activities can increase your likelihood of developing the condition. For example, high-impact sports such as running, basketball, and dancing can put a lot of stress on your feet. This repetitive impact can gradually wear down your plantar fascia.
In addition, if you suddenly increase your activity, such as starting a new exercise program, your feet may not be able to handle the increased load, leading to strain. Standing or walking for long periods of time can also strain your foot muscles and ligaments, increasing your risk of plantar fasciitis.
Footwear Choices
The shoes you wear on your feet can have a significant impact on the development or worsening of plantar fasciitis. High heels, while fashionable, can cause the Achilles tendon to tighten, putting more pressure on the plantar fascia. Similarly, shoes without adequate arch support, such as flip-flops or flats, can cause instability and strain on the foot. Even the best running shoes wear out over time, and running in old or worn-out sneakers can lack the necessary cushioning to protect your feet, leading to plantar fasciitis.

Health Conditions
Certain health conditions may predispose you to plantar fasciitis, so it is important to be aware of these risks in order to take preventative measures. For example, obesity can put extra pressure on your feet, causing more stress on the plantar fascia. People with diabetes often have poor circulation, which can negatively impact foot health. Additionally, conditions such as lupus or rheumatoid arthritis can cause inflammation in the feet, increasing the risk of plantar fasciitis.
How to Treat Plantar Fasciitis At Home
Generally speaking, the early stages of symptoms are easy to treat and pain can be relieved at home. However, the longer the symptoms last and the more severe the pain, the longer the treatment time will be, and surgery may even be required.
Stretching and Physical Therapy
Stretching is one of the best ways to treat plantar fasciitis. Concentrating on stretching the plantar fascia and Achilles tendon, a physiotherapist can show you some stretching exercises that you can repeat several times a day at home. These exercises can also strengthen the calf muscles and help stabilize the ankle.

Ice and Medication
Apply an ice pack to the affected area for 15-20 minutes several times a day, as well as over-the-counter pain medications (such as ibuprofen or aspirin) to reduce pain and inflammation. Your doctor may also recommend NSAIDs to reduce discomfort.
Rest, Activity Modification, and Orthotics
It is important to reduce weight and pressure on the foot while the plantar fascia is healing. Choose shoes with good arch support and cushioning and avoid high heels and flip-flops. Perform regular stretching exercises, especially for the calf and plantar fascia. Minimize prolonged standing or walking on hard surfaces and maintain a healthy weight to reduce pressure on the feet. The use of customized orthotics can provide additional support and relieve pressure on the plantar fascia.
Long-Term Management Approach
Long-term management of plantar fasciitis requires consistent measures to prevent recurrence. Continue regular stretching and strengthening exercises to maintain flexibility and strength in your feet. Adjust your activities to avoid putting undue stress on your feet by choosing low-impact exercises such as swimming or bicycling.
Always wear proper footwear, even at home, and consider rotating between shoes to avoid excessive wear. Control your weight to reduce pressure on your feet and consider using a night splint to keep your plantar fascia stretched while you sleep to reduce morning pain.
If your symptoms are so severe that treatment at home is no longer sufficient, you need to refer to the following methods.
Shockwave Therapy
Shockwave therapy promotes healing of the plantar fascia by emitting low- or high-energy shockwaves into specific areas, causing micro-trauma, which triggers the body's healing response.
While medical interventions such as corticosteroid injections reduce inflammation and pain, shockwave therapy uses sound waves to stimulate healing. In severe cases, surgical intervention may be required to release tension in the plantar fascia.
Surgery
In severe cases, surgery may be an option. Gastrocnemius recession or gastrocnemius release surgery is aimed at lengthening the gastrocnemius tendon and relieving the connection between Achilles tendon tension and plantar fascia tension. This procedure is often recommended for patients who are unable to hold their foot in a neutral position due to tight calf muscles and tendons.
What are the Best Socks And Shoes for Plantar Fasciitis?
Effective treatment of plantar fasciitis requires wearing the right socks and shoes. The right shoes can significantly reduce discomfort and promote healing.
Best Socks for Plantar Fasciitis
- Compression Socks: Compression socks provide extra support and improve circulation, helping to reduce inflammation and pain. They stabilize the foot and prevent further pressure on the plantar fascia.
- Support Socks: Look for socks with extra cushioning, especially in the heel and arch areas. This extra padding absorbs shock and reduces pressure on the foot, providing much-needed comfort.
- Moisture-Wicking Socks: Moisture-wicking socks made from synthetic fibers or wool help wick sweat away from the skin, keeping your feet dry. This prevents blisters and reduces friction, which can worsen plantar fasciitis symptoms.
- Seamless Socks: Socks with a seamless design can reduce friction and irritation, especially when worn for long periods of time. This can help prevent blisters and discomfort and is ideal for those with sensitive feet.

Best Shoes for Plantar Fasciitis
- Supportive Running Shoes: Running shoes with good arch support and cushioning are very effective.
- Orthopedic Shoes: Orthopedic shoes are designed to support foot health.
- Shoes with Removable Insoles: Shoes with removable insoles allow you to insert custom orthotics that provide tailored support. This feature is especially beneficial for people with special foot needs.
- Shock Absorption. Choose shoes with good shock absorption, especially in the heel area. Cushioned soles or gel insoles can help absorb shock.
Conclusion
Identifying early symptoms like heel pain and stiffness can help manage the condition effectively. Simple measures like rest, wearing the right shoes and socks, and stretching can make a huge difference if caught early. Ignoring the pain can lead to more serious problems that may require medical attention.
If symptoms persist, seek professional help immediately. From physical therapy to medical intervention, there are effective treatment options available to help you get rid of the pain.
Related more:
Are Compression Socks Good for Diabetes?