Elevated blood sugar levels, commonly known as blood glucose, can damage the nerves in the feet, leading to a condition known as diabetic neuropathy. This nerve damage can cause a loss of sensation, making it difficult to feel injuries or pressure points on the feet. Additionally, diabetes affects blood circulation, reducing the supply of blood to the feet. Without proper blood flow, wounds and ulcers may have difficulty healing, increasing the risk of infection.

What Are the Symptoms of Diabetic Foot Pain
Due to a combination of poor circulation and nerve damage, diabetes can lead to a variety of foot problems. Identifying these symptoms early can help prevent serious complications. Common symptoms of diabetes-related foot problems include:
- Numbness or tingling: Common symptoms of nerve damage (neuropathy), resulting in a loss of feeling in the feet.
- Pain or burning sensation: Even minor injuries can cause significant discomfort due to nerve damage.
- Swelling: Persistent swelling in the foot or ankle may indicate an underlying problem.
- Redness or warmth: Signs of infection or inflammation, especially around wounds or sores.
- Sores or ulcers: Wounds don’t heal properly and can become infected.
- Changes in skin color or temperature: Indicates poor circulation or infection.
- Cracked or dry skin: This leads to an increased risk of infection.
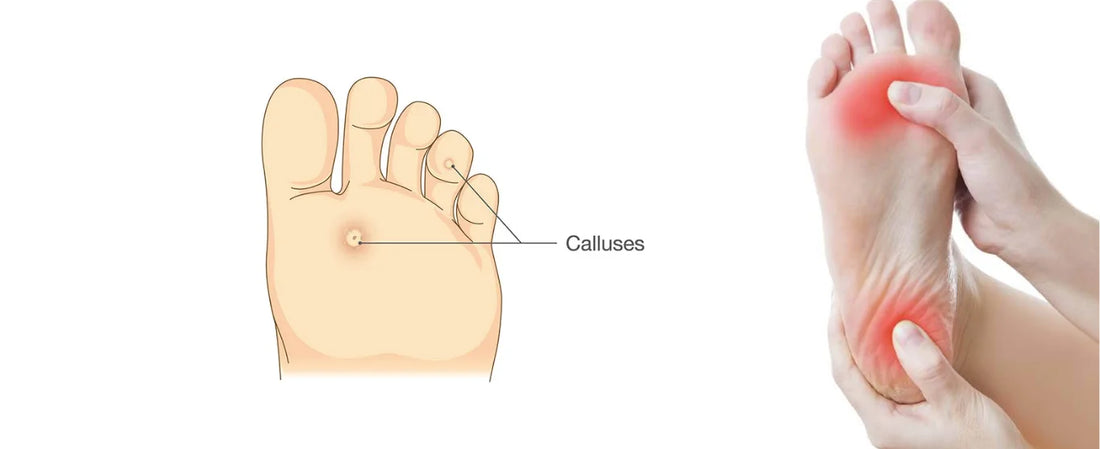
- Corns and calluses: Due to pressure points on the feet, these thickened areas of skin can lead to ulcers if not treated promptly.
- Fungal infections: Conditions such as athlete’s foot and toenail fungus are more common in people with diabetes and are more difficult to treat, which can lead to further complications.
- Ingrown toenails: People with diabetes are more susceptible to infections, which can lead to more serious problems if left untreated.
- Hammer toes and bunions: Structural deformities can lead to pressure points and ulcers, requiring proper footwear and sometimes surgical intervention.
Why Do Diabetics Have Foot Issues?
Diabetes is a chronic disease that affects how the body uses blood sugar (glucose). Glucose is the body's main source of energy, but in people with diabetes, blood sugar levels are elevated due to insufficient insulin or the body's inability to use insulin effectively. Chronic high blood sugar can lead to a variety of complications, including nerve damage and blood vessel disease.
Related read: How To avoid developing type 2 diabetes
Peripheral Neuropathy
Diabetes can cause nerve damage, particularly in the feet, leading to a condition known as diabetic neuropathy. This results in decreased sensation, making it difficult to feel pain, heat, or cold, so injuries or sores may go unnoticed and untreated. Neuropathy can also affect the muscles of the feet, leading to deformities such as hammertoes or Charcot's foot, creating pressure points that can result in calluses and ulcers.
Poor Blood Circulation
Diabetes can lead to peripheral arterial disease (PAD), where the blood vessels become narrowed or blocked by fatty deposits, reducing blood flow to the feet. This impairs the body’s ability to heal wounds and fight infections, causing the feet to feel cold and slowing down the healing process for cuts, blisters, or sores.

Increased Risk of Infections
High blood sugar levels can weaken the immune system, making diabetics more susceptible to infections. The combination of neuropathy and poor circulation can lead to the development of foot ulcers, which are prone to infection due to impaired immune response and delayed healing. In severe cases, untreated infections can lead to tissue death (gangrene), potentially necessitating amputation to prevent the spread of infection.
Foot Deformities
Charcot foot is a serious condition involving the weakening of bones in the foot, which can occur in people with significant nerve damage. The bones are more likely to fracture and, with continued walking, the foot can change shape. Early intervention is crucial to manage this condition.
Calluses and Corns
Abnormal foot structure and gait can lead to increased pressure points on the feet, causing calluses and corns to develop. If not managed properly, these can lead to ulcers. Diabetics often have thicker skin on their feet, which can crack and become infected more easily.
What Can I Do to Keep My Feet Healthy?
Caring for your feet is crucial in avoiding serious foot complications, especially when you have diabetes. Here are detailed steps to help you keep your feet healthy:
1. Wash Your Feet Thoroughly Every Day
Clean your feet with warm (not hot) water and mild soap daily. Make sure to wash all areas, including between your toes, to remove any dirt and bacteria.
2. Dry Them Thoroughly
After washing, dry your feet completely, paying special attention to the areas between your toes. Moisture left between your toes can create an environment conducive to fungal infections.
3. Wear Moisture-Wicking Socks
Choose socks made of moisture-wicking materials, such as specialized athletic socks, breathable cotton socks, plus size compression stockings. This helps keep your feet dry and reduces the risk of fungal infections.
Related read: Are compression socks good for diabetes?
Compression socks apply gentle pressure to your legs and feet, which can help improve blood flow. This is especially helpful for people with diabetes who have peripheral artery disease or are at risk for blood clots.
Compression socks can help reduce swelling in the feet and ankles, a common problem for people with diabetes who have circulation issues. But it’s best to consult your healthcare provider to choose the right level of compression for your specific needs.

4. Moisturize Your Feet
Apply a good quality moisturizer to your feet to keep the skin soft and prevent cracking. However, avoid applying lotion between your toes, as this can encourage fungal growth.
5. Keep Your Toenails Trim
Regularly trim your toenails straight across to prevent ingrown toenails, which can become infected. Use an emery board to smooth any sharp edges that might catch on socks or shoes.
6. Check Your Feet Daily
Inspect your feet every day for any signs of sores, cuts, blisters, corns, or redness. Use a mirror to check the bottoms of your feet if necessary. Report any abnormalities to your doctor immediately to prevent complications.
7. Check Your Shoes Before Wearing Them
Before putting on your shoes, inspect the insides for any sharp objects, small rocks, or debris that could injure your feet. Even small objects can cause significant problems if unnoticed.
8. Wear Well-Fitting Shoes
Ensure your shoes fit properly and do not rub or pinch your feet. Shoes that are too tight or loose can cause blisters, calluses, and other foot issues. Consider getting shoes specially designed for diabetics, which provide extra support and protection.
While You’re At It, Avoid These
- Don’t Walk Around Barefoot
Always wear shoes or slippers, even indoors, to protect your feet from injuries and infections. Walking barefoot increases the risk of cuts, punctures, and other injuries that can lead to serious complications.
- Don’t Soak Your Feet
Avoid soaking your feet for long periods, as this can lead to dry, cracked skin. Prolonged exposure to water can strip away natural oils, making your skin more vulnerable to infections.
- Don’t Smoke
Smoking impairs circulation and reduces blood flow to your feet, exacerbating the risk of foot problems. Quitting smoking can significantly improve your overall health and reduce complications related to diabetes.
Additional Tips for Foot Health
- Regular Check-Ups
Schedule regular check-ups with a podiatrist or healthcare provider who can monitor your foot health and address any issues early on.
- Proper Footwear
Consider custom orthotics or diabetic shoes that provide extra cushioning and support to reduce pressure points and prevent foot injuries.
- Blood Sugar Management
Maintaining stable blood sugar levels is crucial in preventing nerve and blood vessel damage. Work with your healthcare team to manage your diabetes effectively.
- Stay Active
Regular physical activity can improve circulation and overall health. Choose low-impact exercises like walking, swimming, or cycling to keep your feet in good condition without putting too much strain on them.
- Educate Yourself
Learn about the signs and symptoms of foot problems related to diabetes. Being well-informed helps you take proactive steps to prevent complications.
By following these detailed steps and making foot care a daily routine, you can significantly reduce the risk of serious foot problems and maintain better overall health as a diabetic.